A Complete Guide to Intestinal Permeability: What It Is, Why You Have It, And How to Support It
More people have reported an inability to digest certain foods and an increase in seemingly unexplainable intolerances and sensitivities. I’m not just talking about dairy and gluten; I’m talking about the indigestion of specific macronutrients (i.e., fats, proteins, and carbohydrates). Does this sound like you?
Aside from growing increasingly sensitive to the foods we’re eating, there has also been quite an increase in autoimmunity. While these two ‘unrelated’ happenings have been increasing in presence, they—and a ton of other ‘modern maladies’—have a lot more in common than you might think: intestinal permeability. Intestinal permeability and autoimmune disease tend to go hand in hand, and I believe it’s one major roadblock keeping many people from getting well again.
WHAT IS INTESTINAL PERMEABILITY?
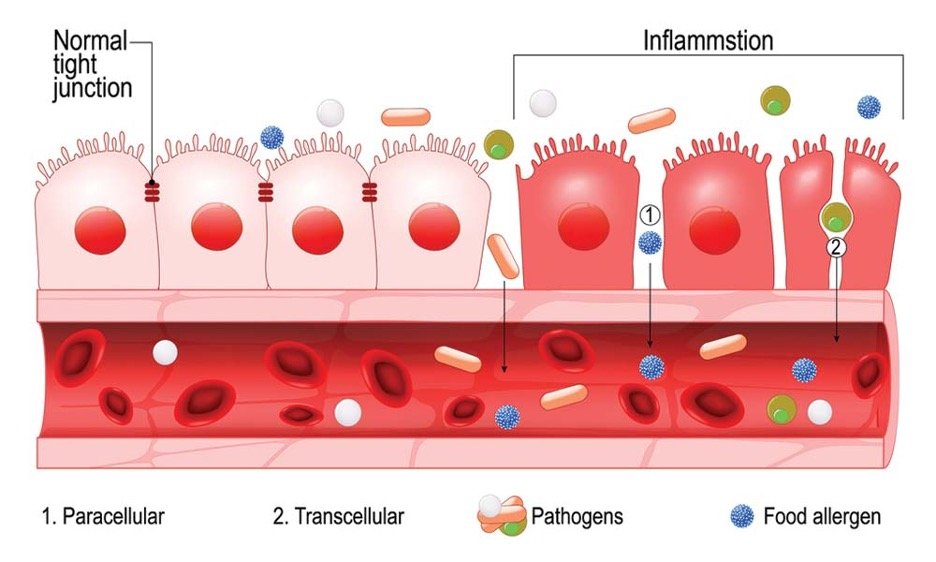
When we refer to intestinal permeability or “leaky gut,” we’re talking about the occurrence of maldigested foods making their way into the bloodstream, where they are recognized as an antigen. This can ignite the immune system, trigger an inflammatory cascade, and lead to a TON of problems. Don’t worry; we’ll explain it all in detail below!
Intestinal permeability meaning foods are making their way into the bloodstream, thus activating inflammation.
In this article, I want to talk about the inability to digest certain foods or food groups due to intestinal permeability, intestinal permeability symptoms, some intestinal permeability causes, and how to support it. I also wanted to use this as a lead-in to address more “niche” sensitivities like lectins, thiols, and oxalate in my next post. If you’ve never heard of them, these are plant compounds known as “antinutrients” that could be contributing to your “mystery” food sensitivities.
Check out that blog post, Ill Digestion, Leaky Gut, and Deteriorating Effects of Antinutrients here!
TABLE OF CONTENTS:
Intestinal Permeability Symptoms
How Does Digestion Work? Digestion Is a North to South Process
What Can Cause Leaky Gut Syndrome, or What Causes Intestinal Permeability?
How to Heal Intestinal Permeability: Improve Protein Digestion
How to Heal Intestinal Permeability: Improve Fat Digestion
How to Heal Intestinal Permeability: Optimize Pancreatic Function
Is There an Intestinal Permeability Diet?
The Basics: What 3 Foods Cause Leaky Gut?
What About Supplements to Heal Me?
Dysautonomia or Nervous System Dysfunction
Recognizing The North to South Function
Working with a Nutritional Therapist
INTESTINAL PERMEABILITY SYMPTOMS: A CASE STUDY OF YOURS TRULY
Now… onto a bit of anecdote from my situation! As a sophomore in college, I was anxious and depressed, my bowel habits switched from having to make a break for it to needing a pot of coffee to get things moving, and I couldn’t sleep through the night to save my life. I had massive craters on my chin and forehead that I now know were from imbalanced hormones and a GI tract that was screaming for attention.
Aside from what I’ve listed, you might also experience (these are not causes) things like:
- Intolerances to specific foods or reactions that seem unpredictable;
- Constipation where you have to grab laxatives (yes, coffee counts);
- Unexplained, un-ending diarrhea;
- A mixture of both;
- Seasonal (airborne) allergies;
- Mood disorders like anxiety or depression;
- Chronic fatigue syndrome (CFS);
- Chronic pain of fibromyalgia;
- Candida;
- Small Intestinal Bacterial Overgrowth (SIBO);
- Lyme disease;
- Parasites;
- Poorly digested food in stools;
- Bloating;
- Hormonal imbalances like PCOS, endometriosis, amenorrhea, or infertility;
- Unexplained weight gain or loss;
- Fatigue, inexplicable tiredness, the need to sleep a lot;
- Vitamin and mineral deficiencies or imbalances (low OR high);
- Problems concentrating and conditions like ADD, ADHD, or autism;
- Skin problems like acne, eczema, or rosacea; and
- General feelings of unwellness.
Although it isn’t a formal “Do I Have Leaky Gut Quiz,” you can likely infer that you probably have some degree of intestinal permeability if a good chunk of these symptoms applies to you.
It’s all connected.
Aside from symptoms, there are also tests you can use in conjunction with a qualified health practitioner that can help you confirm your symptoms. An intestinal permeability assay looks at things like zonulin, enzyme function, microbial balance, and how well you’re digesting and absorbing your foods. Labs like Genova Diagnostics or Great Plains Laboratory have great, in-depth stool analyses. You do need a practitioner to order one, and it can be helpful to have one interpret it for you. They can be confusing. The intestinal permeability test cost is also quite high, making it tough to run or run consistently.
A Genova intestinal permeability test sample report. I am not affiliated aside from interpreting and using within my practice.
Similar to how most successful civilizations built themselves around a flowing, roaring body of water, the gastrointestinal system is a ‘tube of life’ from the outside world running through your insides to bring vitality. If it’s unhealthy, you’re putting harmful things in it, or you’re not taking care of it, it’s easy to see—with this analogy, anyway—that the ‘life’ around it might not be so… well, lively. We’ll get to why that is in a minute.
HOW DOES DIGESTION WORK? DIGESTION IS A NORTH TO SOUTH PROCESS
To understand how we can end up with a leaky gut, intestinal permeability, and gastrointestinal dysfunction, we need to understand the process of digestion. Then we can analyze how ordinary happenings tend to cause and contribute to it.
Digestion begins—literally—at the sight of food. When we’re about to eat, our hypothalamus communicates that salivation needs to occur to the rest of our bodies. Why? Within our saliva is water, yes. But another part of it is salivary amylase, an enzyme used to break down carbohydrates like starches. With the help of saliva, teeth, and tongue, we “masticate” our food into a “bolus” to move into the stomach for the next step of digestion. If you’re not chewing your food correctly—thirty to thirty-five bites—you’re not doing your digestion any favors. Slow your roll and chew and savor!
The bolus is squeezed and transported by the esophagus and into the stomach via the esophageal sphincter. This sphincter serves as a “safety door” between the esophagus and the stomach. Once in the stomach, chemical digestion continues. Hydrochloric acid—in a healthy being—is released, lowering the pH to between 1.5 and 3.0. Keep in mind: 7 is neutral. When pH is below seven, it is increasingly more acidic. When it is above seven, it is increasingly more basic. Here, we want pH lower to break down the bolus further.
If stomach pH is not adequate, we can see acid reflux. The esophageal sphincter closes once the pH reaches a particular acidity (between ~1.5 and 3.0) and will not close if the pH is too high. This acidic bolus comes back up with GERD and acid reflux as a result. This means stomach pH is TOO weak. In conventional medicine, we see acid blockers and PPIs prescribed to “lower stomach acid”…*shaking my head*. These drugs do this successfully but to your detriment.
First and foremost, hydrochloric acid is an essential antimicrobial to bacteria like H. Pylori. Prolonged use can set you up for a whirlwind of problems. True hyperacidity is rare, and these drugs just exacerbate HCL insufficiency. Second, your body needs stomach acid to break down your food and absorb it properly. This is perhaps the most essential part! Without adequate stomach acidity, you’re not getting the nutrients you require to make stomach acid, rebuild your body, mount an immune response, and stay healthy. Finally, it’s not unlikely for someone to have to take more and more antiacids to suppress this acid production. This is literally your body trying to overcome the obstacle you’ve put in front of it to digest food successfully! The more you take, the more you’ve blocked your own function.
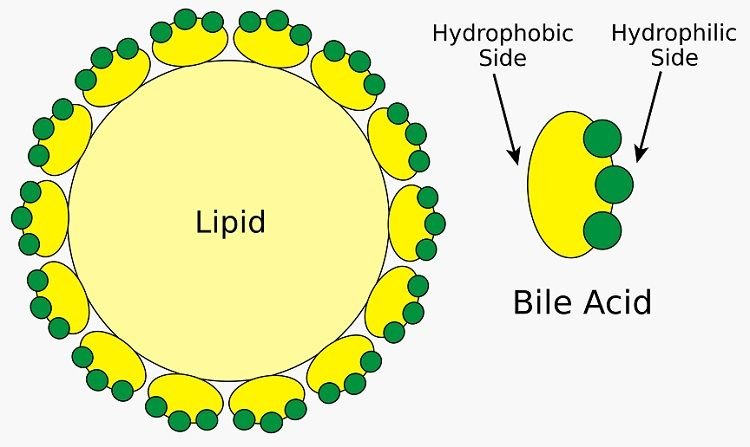
If the pH is correct and sufficiently acidic, something known as pepsinogen is activated. Pepsinogen begins the breakdown of protein. This mixture of food, hydrochloric acid (HCL), and pepsinogen is now known as chyme. From here, the chyme moves through the pyloric sphincter and into the first part of the small intestine, known as the duodenum. Here, it remains at a pH of 1.5-3.0, and something known as secretin is released. Secretin then forces the release of sodium bicarbonate. At this point, the pH is neutralized, and another substrate is released: cholecystokinin (CCK). CCK leads to bile secretion from the gallbladder and various enzymes from the pancreas to continue the chemical breakdown of fats and proteins.
So we can summarize these reactions here…
1. Without HCL and a pH of 1.5-3.0 in the stomach:
Pepsinogen will not be released to digest proteins.
Food will not be released into the small intestine.
Secretin will not be released in the small intestine.
2. Without the release of secretin, sodium bicarbonate will not be released.
3. Without the release of sodium bicarbonate, cholecystokinin (CCK) will not be released.
4. Without the release of CCK, bile and pancreatic enzymes will not be released.
(in short, you will not be breaking down or absorbing the nutrients in your food and will put yourself at risk for increased intestinal permeability)
Keep this summary in mind as we continue this discussion.
Bacteria is also present throughout the GI tract to help ferment, break down, absorb, and even produce nutrients from the foods you’re eating. They’re also present to defend you from harmful bacteria that you can bring into your GI tract from eating, drinking, or breathing subpar food, water, or air. And yes, we all do it to some degree!
As these components break down, they’re mostly absorbed and assimilated by the small intestine (mainly in the first section known as the duodenum). That is, in a healthy individual. The lining of your small intestine is lined with a thin layer of cells known as enterocytes. These cells are super absorptive and absorb all the nutrients you’re consuming from food and get them into your bloodstream. In essence, their health is vital for yours!
Aside from only being one layer thick, these enterocytes are also tied together via something called gap junctions. Essentially, these junctions work like glue and ensure that nothing seeps in between them to make it into your bloodstream unannounced.
Around 60% of your immune system lies on the other side of the “barrier” known as your intestines and within gut-associated lymphoid tissue (GALT) throughout your intestinal tract. It makes a lot of sense, considering your gastrointestinal tract is a “tube from the outside” making its way through you. Anyway, your gap junctions and enterocytes play the role of security guards around a junkyard (and yes, this analogy is essential) that are trying to keep transport into your body organized and in check. If your gap junctions start to fall apart, food starts to seep in without any check or balance, just like an intruder. Once these intruders are running around, your “junkyard dogs” (your immune system) turns on and sets off in search of whatever has made its way in.
Is it flour from chicken nuggets? Some soybean oil from those McDonald’s fries? Maybe it’s even those paleo sweet potatoes you air fry and cook EVERY DAY, but they’ve made it into your bloodstream SO MANY TIMES, you’re now sensitive to them. Nonetheless, this is where the link between intestinal permeability and autoimmunity (or leaky gut and autoimmunity, whichever you prefer) exists; once the immune system is activated from the “assault” it’s experienced from eating these foods that are making it into the bloodstream, it can “mistake” them for tissues like your thyroid (Hashimoto’s), collagen (Ehler’s Danlos), connective tissue (Lupus), and nervous system (Multiple Sclerosis) in a process known as molecular mimicry.
Source: https://creativemeddoses.com/topics-list/molecular-mimicry-in-guillain-barre-syndrome/
Once this digested matter proceeds through the rest of the small intestine, it passes through the ileocecal valve and into the large intestine. Here, minerals and water from food are absorbed, and the remainder is excreted as waste.
It’s important to keep in mind that nutrient absorption happens throughout the gastrointestinal tract. For this reason, it’s critical to optimise the function and health of the entire thing, and to support it to '“do its thang”all the way through! I’ve included a cool chart to outline where different nutrients are primarily absorbed.
Now that you understand the series of reactions needed to take place for digestion, it’s time to analyze the dysfunction.
WHAT CAN CAUSE LEAKY GUT SYNDROME, OR WHAT CAUSES INTESTINAL PERMEABILITY?
If we were to think of an assembly line, any inefficiency in one worker would block up the line. Your digestion is no different! We're stopping digestion straight out the gate if we’re not chewing or masticating our food. If we’re halting the flow of any digestive juices—whether it be stomach acid, bile, or pancreatic enzymes—we’re impeding digestion somehow. And, if we’re killing off the bacteria with antibiotics, antifungals, or even herbs, we could be decreasing how efficiently we can break foods down and absorb them. Interestingly enough, stress on the body—whether it be emotional, mental, biochemical (nutrition), or physical (like too much exercise)—can also interrupt our GI function. That’s explained in my blog post detailing adrenal dysfunction, stress, cortisol, and all things in between. Thus, we could say that intestinal permeability can result from:
Antibiotic overuse (or use at all, if someone is immune-compromised during the time they’re administered);
Antifungal overuse (or use at all, if someone is immune-compromised during the time they’re administered);
The use of certain pharmaceuticals, like proton pump inhibitors (PPIs, because they inhibit stomach acid production), bile-stopping drugs like birth control, estrogen, or certain antibiotics;
Psychosomatic stress;
Overexercise;
Long-term nutrient deficiencies, as we require nutrients to produce and synthesize stomach acid, pancreatic enzymes, and bile acids responsible for digestion and emulsification of foods;
Consuming processed foods that are full of gluten, corn, soy, associated pesticides, and sugar;
Drinking abrasive beverages like alcohol, soda pop, and coffee (for some) as these products produce the perfect environment for microbes to fester;
Dysbiosis from bacterial or fungal overgrowth, as these microbes are known to breakdown the tight gap junctions between enterocytes;
Impaired stomach function, biliary function (gallbladder or liver disorders), or pancreatic function (pancreatitis);
Systemic infections like Lyme Disease or other Lyme coinfections can cause inflammation that works similarly;
Excessive use of NSAID pain relievers or other anti-inflammatories like Advil, Tylenol, or Naproxen, as these drugs downregulate the production of enzymes that produce substances like mucus that protect your GI tract from its own acidity and enzymes;
Consuming toxins like heavy metals, mold (from the environment or food), bisphenols, dioxins, phthalates, or microbes from drinking unfiltered water, food, or air; or
A combination of all of the above, especially for extended amounts of time (chronic).
Looking back on my personal situation, it was definitely a “perfect storm” combination of all of the above, and I can attribute my onset of leaky gut to a series of unfortunate events. You see, my steady downhill of college wasn’t my first run-in with illness. When I was eleven, I actually had missed a solid year from something similar. After experiencing extreme pain from gastric spasms that no doctor could explain, I made my rounds to the University of Chicago, Rush University, Loyola, and some of the region’s “best.” Still, no answers. I did countless rounds of antibiotics, muscle relaxers, and IBS drugs. I tested positive for 78 food sensitivities and saw every world-renowned chiropractor, Chinese medicinist, acupuncturist, and gastro MD in the tristate area. Interestingly, it coincided with a ton of family issues. Once they improved (for the time being), I did, too.
With regard to college, I can attribute it all to being highly stressed from a destructive family dynamic, running a ton, an unhealthy romantic relationship, and taking a full load at university. I also didn’t have a suitable living situation (emotionally or environmentally). I only ate lean protein, vegetables, some fruit, and a ton of sugar-free whatever to keep my calories and carbs low. To top it off, I had had hip surgery a few months prior and had been on and off antibiotics and opioid pain medicine. This undoubtedly increased intestinal permeability symptoms.
I decided to jump to veganism because protein was no longer sitting with me, which helped at first. I ate massive amounts of rice, beans, pasta, fruit, and vegetables… no fat, no salt, and not much protein! In the short run, this helped my symptoms because it eliminated what my body became incapable of digesting: protein. Note here I did not say I was intolerant of it, but I could not digest it well anymore. By eliminating it, I managed a symptom instead of looking at the root problem. This set me up for many digestive issues further down the line. For perspective, my sophomore year was five years ago, and I'm still dealing with the damage! So, how did I come back from it, and what insight do I have on how to heal intestinal permeability?
HOW DO HEAL INTESTINAL PERMEABILITY: IMPROVE PROTEIN DIGESTION
As we mentioned, the release of pepsinogen in the stomach initiates protein breakdown. This is prompted when the stomach reaches an optimal pH of 1.5-3.0 with hydrochloric acid (HCL). Without proper acidity from HCL, pepsinogen is not activated. Your protein will most likely sit there like a brick in mud. Aside from protein digestion, this reaction is also super crucial for B12 absorption.
So… how do we get our hydrochloric acid up and running? For starters, one of the main components of hydrochloric acid is zinc. We also need B vitamins, iron, water, and salt. If you’re reading this as a vegan or vegetarian—or don’t eat much meat—it’s important to note that there isn’t much bioavailable (absorbable) zinc in plant foods. You might believe it is, but much of it is antagonized by compounds like phytates and oxalates in plant matter. Our most bioavailable and absorbable source of zinc comes from animal products like meats, poultry, fish, and eggs. The longer one adheres to a diet free of these products, the more deficient one becomes in it. Over time, less stomach acid is produced. It’s a vicious cycle: if someone isn’t making enough stomach acid, they’re also unable to break down the zinc-rich protein they are consuming to make more HCL. Kind of upsetting, isn’t it? It was for me.
The production of HCL also is reliant on something else: stress. The parasympathetic nervous system is needed for the “rest and digest” processes to commence—this includes the proper production of HCL. The sympathetic nervous system—or the “fight or flight” response—becomes activated in times of stress (the body can’t tell if you’re running from a predator to overcome death or stressing about that tax return) and switches to survival mode. Blood is diverted away from the thorax and digestive organs and to the brain and the limbs to get the heck away from a predator! If you’re chronically stressed, your body isn’t putting much energy into digestion—it’s convinced you’re runnin’ from lions. It’s paramount to work on stress management around meals if you’re struggling with any sort of digestive distress.
If you’re already dealing with digestive issues—say malabsorption, improper digestion, or some type of overgrowth like candida, H. Pylori, SIBO, or SIFO—these factors influence the absorption rates of everything: amino acids, fats, carbs, vitamins, and minerals. In this situation, you might not be getting the zinc you think you are.
I could write on about the importance of stomach acid, but the main point of this section was to highlight the importance of analyzing your zinc status, pathogenic burden, and stress levels if you’re having a hard time digesting protein!
HOW TO HEAL INTESTINAL PERMEABILITY: IMPROVE FAT DIGESTION
Let me start off with two questions: do you have your gallbladder, and do you/have you ever followed a low-fat diet? These are two major causative factors in improper fat breakdown, and they don’t take much thought. The liver is responsible for bile production, and the gallbladder oversees storing this fat-emulsifying substance. We hear of people often having their gallbladders removed because of the formation of gallstones. Did you know that gallstones can form from lowered consumption of fats?
Thanks to modern diet culture, we often fear fat like the plague. At nine calories per gram, fat is relatively dense in calories. However, we need it to synthesize bile acids, make hormones (that help you lose weight and feel food), and store and absorb fat-soluble vitamins. It’s also an energy-efficient form of fuel, kind of like human diesel. Fats can become problematic when we eat the wrong types, often in their processed and industrialized forms (ahhhem, seed oils). While it can be easy to go “low calorie” by simply axing fats, you might want to rethink that.
Bile is released into the small intestine—specifically the duodenum—when it’s signaled that fat has been consumed and needs to be digested. If you’re regularly consuming fats, your bile is regularly being filtered out and replaced. Think of fuel coming into your car when you’re regularly driving it: you’re constantly refilling the tank and putting new in. If you’re never consuming fats—as in the low fat/no fat diet—this bile is sitting in your gallbladder waiting to be used (keep thinking about fuel, sitting there for years on end). It eventually begins to form gallstones from stagnation, and you might end up without your gallbladder. Most people avoid fat like the plague if they have gallbladder dysfunction because this already-strained system is being stressed. Remember: gallbladder dysfunction is a symptom! It’s essential to address the underlying issue and thin the bile. Avoiding diets high in processed fats is vital as they’re much harder to break down and emulsify.
Now, if you don’t have your gallbladder, you’re not storing much bile. If you’re eating a heavy amount of fat without a gallbladder, it’s warranted that you probably won’t feel great! You might see some fat within your stool. You might experience constipation, nausea, or diarrhea from not being able to break it down. It’s also possible that you won’t absorb dietary fats for bodily function or that you won’t be adequately absorbing fat-soluble vitamins. These occurrences can happen without a gallbladder and in someone who has a dysfunctional liver and gallbladder. It’s imperative to keep eating fats in the diet and support bile production and excretion. Why? Well, we need fats for a lot of bodily processes. Bile is also one of the main pathways of excretion for blood-filtered toxins, as it releases them into the intestines to ensure these metabolic wastes make their way out through your stool.
Mediating a malfunctioning gallbladder can be done with nutrition support and supplementation—don’t worry! It’ll take some patience and hard work, but it’s within reach.
HOW TO HEAL INTESTINAL PERMEABILITY: OPTIMIZE PANCREATIC FUNCTION
Much of the western diet is reliant upon carbohydrates. This dependence can contribute to digestive dysfunction in another organ critical to food breakdown: the pancreas.
Enzymes break down carbohydrates once food enters the small intestine. What are enzymes, exactly? Enzymes are catalysts—they’re proteins that expedite the breakdown of a substance. Without them, many of the foods that we consume would go undigested. If you can recall, the pancreas—and the salivary glands—produce enzymes. Those made by the pancreas are released into the small intestine after the chemical reactions we touched on earlier.
It’s important to know there are multiple enzymes produced by the pancreas, including:
Proteases, which are responsible for the breakdown of proteins into amino acids. There are two types of proteases known as trypsin and chymotrypsin;
Lipases, which are responsible for the breakdown of fats and lipids. Coupled with bile, these substances allow for the breakdown of fat molecules into monoglycerides that the intestinal tract can readily absorb; and
Amylases, which are responsible for the breakdown of polysaccharides (carbohydrates) into more absorbable molecules, such as monosaccharides like glucose.
There are other enzymes we could touch on (like lactase and cellulase), but I’d like to save them for another post. Let’s examine why you're not releasing OR producing enzymes in the first place.
If we can recall:
HCL = pH of 1.5-3.0 = release of secretin —> sodium bicarbonate —> release CCK = ** the release of pancreatic enzymes **
We need hydrochloric acid to be sufficient to trigger these successive reactions. If HCL levels are adequate, it’s still essential to analyze digestion from start to finish. What could be throwing a wrench in the chain and impeding the release of the others? Let’s jump to examine the health of the pancreas.
The pancreas is a very fragile organ susceptible to conditions known to inhibit its function. In a condition known as pancreatitis, the pancreas can become chronically inflamed. Because of the pancreas’s role in glucose control, chronic and erratic blood sugar can play a part in the onset of pancreatitis. Regular and excessive intake of alcohol, infection and drug use also can contribute to it. Because of this organ’s role in enzyme production, pancreatitis may be a root cause behind your digestive inabilities. If you see particles of plant foods in your stool, have stools that float, are exhibiting signs of hypoglycemia/hyperglycemia, or if you’ve been diagnosed with diabetes, then your pancreas might not be working on all eight cylinders. As a result, it may be predisposed to pancreatic dysfunction and poor enzyme production.
Mediation of pancreatic dysfunction begins with limiting carbohydrates while incorporating more fat and protein into the diet. It often also requires some stress management, considering the adrenal glands go hand-in-hand with how you’re managing your blood sugar. It’s so craaaaazy how everything is connected, isn’t it?!
IS THERE AN INTESTINAL PERMEABILITY DIET?
At this time, there is no universal western medicine intestinal permeability treatment. Unless we figure out how to shapeshift matter, there will never be, and this is because every case of intestinal permeability has a different underlying pathology (or a different cause). While this might have you feeling hopeless, fear not! You can heal your intestinal permeability and comfortably find remission if you can fix or undo some of the underlying causes.
While you might be looking for some type of “Intestinal Permeability Diet,” I hate to break it to you… but it does not exist! While this might sound frustrating, and you may have been persuaded by another blog to believe that an XYZ food list will bring you health and wellness, you’re being led astray, and I’m here to explain why.
For the gut to heal, we must remove everything inflaming it. Your gut cannot recover in an inflaming environment; the two processes cannot go on concurrently. For someone resilient, this might only entail one food—like the fast food you’re treating yourself to on your way home—or switching to filtered water. For someone whose conditions are a bit more progressed, developed, and rooted, this might require a targeted elimination diet for some time to address dysbiosis, repair damage from antibiotic overuse, and supply nutrients while accommodating the foods they cannot tolerate. Take a look at your fingerprint. It is unique to YOU!
Similarly, your diet, lifestyle, stressors, genetics, environment, and everything leading you up to this moment are unique to YOU. While there are general things that you can do to improve your quality of life somewhat, no universal food list will get everyone 100% better. You will still have some things that inflame you that someone else does not and vice versa. However, there are a few universal things that you can do.
THE BASICS: WHAT 3 FOODS CAUSE LEAKY GUT?
While there is no one-size-fits-all, most people seem to see a significant bit of progress by simply removing the three most common allergens from their diets: gluten, corn, and soy (and ingredients derived from these ingredients). Why?
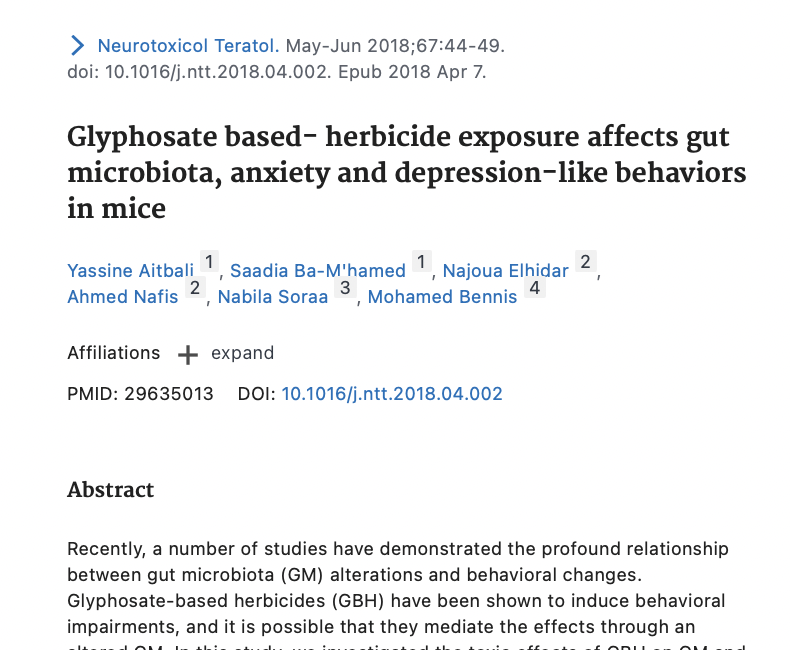
Gluten, corn, and soy tend to be some of the most heavily genetically modified organisms (GMOs). Many experts are still undecided over whether the genetically modified organism itself is a problem. Most argue that it changes the protein structure of the organism, which alters how our gastrointestinal tracts handle it. No matter what you believe on this subject, it’s important to realize that most GMOs are genetically modified to withstand heavy amounts of pesticides, herbicides, and fungicides (like the infamous glyphosate) or produce their own. These pesticides can remain on the foods you’re eating as residues and have been shown in numerous studies to contribute to intestinal permeability directly (by breaking down your gap junctions) and indirectly (by working like antibiotics and throwing off the flora of your microbiome, inhibiting digestive function, and more). Interestingly, glyphosate was patented as an antibiotic in 2010.
Aside from this, traditional preparation of grains like corn, soy, and wheat (gluten) required labor-intensive processes to produce food that was adequately digestible. In other words, native cultures would soak, sprout, ferment, and cook beans, legumes, grains, and other harder-to-digest foods like nuts and seeds to make their nutrients more available. Without proper preparation and with the addition of excessive processing, raw ingredients like corn, wheat, soy, and the proteins inside of them like gluten are challenging to digest. As a result, these proteins go undigested as they pass through your system, especially if your production of stomach acid and pancreatic enzymes is suffering! As they sit on the surface of your small intestine, they become irritated and can compound intestinal permeability.
Gliadin and glutenin are two fractions that come together to create the protein gluten Intestinal permeability is exacerbated by intestinal permeability.
Interestingly, the protein gluten is also known to “mimic” or look like varying human tissues. This is also known as “cross-reactivity,” and it’s a big reason why some people who have a tough time with one grain have a tough time with others. In essence, your immune system is confused with distinguishing between self, antigen (foreign substance like the pizza you just ate), and between antigens. If we put this into practice and consider the link between autoimmunity and intestinal permeability, consuming large amounts of gliadin in the gluten protein tends to resemble thyroid enzymes like transglutaminase. Thus, if they’re finding their way into your bloodstream through a leaky gut, eating gluten regularly can contribute to Hashimoto’s and add fire to a burning Hashi’s flare.
Aside from corn, soy, and gluten, you might consider eliminating white sugar. Not only is most white sugar a product of genetic modification, but it is also straight-up sugar, which is the best thing to grow bacteria and fungus with! Just ask any biologist!!
The best thing you can do if you’re dealing with any degree of intestinal permeability—or to just improve your health, for that matter—is to swap these processed, nutrient-poor foods for nutrient-dense whole foods. Before you go eliminating lectins, oxalates, tannins, alkaloids, salicylates, histamine, dairy, eggs, and whatever else some health influencer might tell you to ax, know that these foods are usually perfectly nutrient-dense foods that can help you heal and that unless you know that you have a problem with them, they should be kept in the diet! Thus, it can take some individual analysis to figure out what can be holding you back.
To learn more about antinutrients and pick up some low oxalate info, check out the post after this one.
WHAT ABOUT SUPPLEMENTS TO HEAL ME?
If you search google for “what can heal intestinal permeability fast” or “heal leaky gut fast,” you’ll find yourself on a wild goose chase reading about other related search terms that pop up, like “collagen intestinal permeability,” “glutamine intestinal permeability,” marshmallow root, slippery elm, and whatever else is hot on the market.
I’m here to hit you with another painful truth: while supplements can help you get better and work as an adjunct, they are by no means a replacement for a healthy, nutrient-dense diet. If we were to liken you to a house with a wobbly foundation, we would by no means just dump a bucket of concrete on it if we saw some cracks. Taking collagen, glutamine, or something similar is kind of the same thing; while your foundation might have some collagen or glutamine in it, it is by no means all there is to it. However, consuming an array of essential micronutrients from foods like animal protein is.
On another note, simply taking collagen to improve your collagen doesn’t always work. Our bodies prioritize the proteins we give them where it needs them most, and we need an array of vitamins, minerals, amino acids, and essential fatty acids to execute human metabolism and actually heal a permeable GI tract. In other words, we don’t have much of a say in where things are allocated, and there is more to what we need to heal than just one processed can of beef in a jar.
DYSAUTONOMIA, OR NERVOUS SYSTEM DYSFUNCTION
There is another factor that we could factor into the mix of faulty digestion, which is the dysfunction of the nervous system. If you’ve experienced head trauma of any sort, your body could be improperly communicating with your organs and their functions indigestion. Post-Traumatic Stress Disorder (PTSD) and Chronic Post-Traumatic Stress Disorder (CPTSD) can have similar effects. These can also arise from living in mold or chronic toxicity of something like heavy metals. Again, this will be a topic of a future post… and I’ll link it here once it’s written.
RECOGNIZING THE NORTH TO SOUTH PROCESS
I hope this post has given you a place to start if your digestive issues can be identified as any of the issues discussed. I really wanted to note the chain of steps necessary for digestion and how one event is reliant on those preceding it. It could be said that digestion is a “north to south” process and that it’s vital to address processes “upstream” before dealing with problems “downstream.” Sometimes, by addressing step #1—like slowing the rate at which you chew your food or (if that’s not a problem) adding hydrochloric acid—the rest of the issues will resolve. And sometimes, it’s a bit more complicated… kind of like a freakin’ 5000-piece puzzle of a scene with 97 shades of green.
WORKING WITH A NUTRITIONAL THERAPIST
It’s easy to demonize the things that we know cause us situational pain and find reasons to justify eliminating them instead of looking a bit deeper at why these foods are a problem. This is your body’s way of telling you where to look at what’s wrong—it doesn’t always mean these foods are your enemies! With all of the misinformation on the web today, it’s also hard to figure out what (nutritionally) is right, what is wrong, what we should avoid, what we should include, and how to fix most digestive disorders …especially on your own!
If you’re working with a nutritional therapist, reach out to them about supporting your system specific to you. Do NOT supplement with a ton of ox bile, pancreatic enzymes, or other digestive supplements without guidance. You can develop dependencies on some of these supplements if you’re not careful and cause more problems down the road when you try and get off of them! If you’re looking for some guidance, shoot me a message. It’s hard sometimes looking at your own case, and it’s hard doing a ton of self-directed research. Consult with a professional to get your health on board for your bio-individual self.
OTHER SOURCES
Wright, Jonathan V., Lenard, Lena. Why Stomach Acid Is Good for You: Natural Relief from Heartburn, Indigestion, Reflux and GERD.
Tortora, Gerard J., Derrickson, Bryan H. Introduction to the Human Body.
Learn True Health Podcast, Episode 333: The Resonance Effect – Part Two. https://www.learntruehealth.com/the-resonance-effect-part-two/
Barclay, Tim. Gallbladder. https://www.innerbody.com/image_digeov/dige04-new.html
Dr. Kellyann. History of Gallstones? Then Say Yes to Dietary Fats! https://www.drkellyann.com/have-a-history-of-gallstones-then-say-yes-to-dietary-fats/
Branney, Peter. https://www.livestrong.com/article/546180-pancreatitis-and-taking-digestive-enzymes/. Pancreatitis and Taking Digestive Enzymes.
The Editors of Encyclopaedia Brittanica. Cholecystokinin. https://www.britannica.com/science/cholecystokinin
Identify EPI. What conditions are associated with EPI? https://www.identifyepi.com/what-is-epi/associated-conditions